SUBJECTIVE ASSESSMENT
What to expect & why
I always think of a physiotherapist as being a detective of the body. An analogy may help to clarify this point.
If a man has been murdered, statistically speaking, the wife is the most likely suspect. If on questioning the wife doesn’t have an alibi and they had recently had an argument this may be sufficient evidence to consider her guilty. We then have a choice, we can either choose to look at evidence that supports this hypothesis or more correctly we can critically evaluate all the evidence and base our decision on the weight of the evidence. We as health practitioners must disprove the guilt of every other structure until we can accurately diagnose the offending structure.
So how do we gather the evidence?
This will start with the consent form in the waiting room that asks you about your relevant medical history. When we see you we may ask a few questions regarding your general health or family health history. These give us added information so we can keep you and us safe with the treatment we provide. Certain conditions such as diabetes or vascular problems can have an effect on healing rates and this helps us set realistic goals and expectations for your rehabilitation.
Then we need to know about where your pain is and how it behaves.
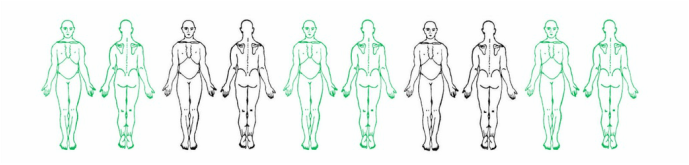
Body Chart
- Location and distribution of your symptoms – do they feel familiar, have you had pain like this before?
- What sort of symptoms – pain, pins & needles or numbness?
- Type of pain – ache, burning, throbbing, catch, stretch: Lets us know the likely structures at fault
- Are the symptoms constant or intermittent?
- How bad is it on a scale of 1 to 10?
Aggravating and Easing Factors
This gives us information about what structures are most likely stressed or damaged and also gives us ideas on what might work for treatment
How easily the symptoms are aggravated and how long they take to settle down guides how vigorous or gentle the treatment can be
24 Hour Behaviour
Such as whether it is worse in the morning, better or worse as the day goes on, whether and how it is disturbing your sleep, or just activity dependant gives us information about whether the pain is primarily mechanical or has an inflammatory component. This will determine how much we think we can help vs the need to refer you to your GP for some medication
Special Questions
We also ask some questions which help us rule out “nasties” or tell us you need to see a doctor rather than a physio – things like sweating at night (not just because you forgot to turn off the electric blanket), recent unexplained weight loss, problems with speech or swallowing or changes in bladder or bowel function. We will also ask you about what medication you are taking and why and whether you have had any scans or not
Current History
How did you hurt yourself or how and when did your symptoms start? Was there a traumatic event, did the symptoms come on gradually? Did anything about your training or lifestyle change prior to the onset of symptoms? How have they changed since they started – are they getting better or worse? Have you had any treatment to date and has it helped?
Past History
This can be very useful. Have you had similar problems in the past? How did they respond to treatment? Do you have a history of symptoms only affecting 1 side. If this is the case we will not only look at where it hurts but further up or down to try and determine why this is happening
Social History
What do you spend your days doing both at work and out of work time – posture, activity, work and home physical environment, as well as stress – all, help us determine how best to manage your symptoms and what may be contributing to them. It also helps us understand more about you and where we need to get you back to (or away from!!)
Goals
This leads into the discussion about where you want to be (within reason…) and what you want to achieve in what time frames. Is there an event coming up that you are training for!
All this information is used to help us develop a working hypothesis and then do the physical testing to prove or disprove this hypothesis.
References
- Petty NJ, Moore A.P. Principles of Neuromusculoskeletal Treatment and Management. A Guide for Therapists (2004) Churchill Livingstone Edinburgh
- O’Sullivan, P. (2012). It’s time for change with the management of non-specific chronic low back pain. British journal of sports medicine, 46(4), 224-227.
- Sizer P.S., Brismee J.M., Cook C (2007) Medical Screening for red flags in the diagnosis and management of musculoskeletal pain. Pain Practice 7(1) 53-71